September 28, 2022
On Depression: Behavioral Activation and Evaluation Criteria
By Emory Strickland, PsyD
FROM EMORY STRICKLAND
Throughout my doctoral training and postgraduate clinical work, I worked with many depressed clients using skills and techniques from Acceptance and Commitment Therapy (ACT) and Cognitive Behavioral Therapy (CBT). Each and every person is different, and there’s no one-size-fits-all approach to overcome depression. For some clients, I focus more on helping them change their thoughts and interpretations about the world. For others, we focus on getting them engaged with daily activities. For many, depression is a manifestation of things not going right in one’s life, and therapy is focused on fixing that problem—such as being in an emotionally abusive relationship or being unhappy in your career.
Depression differs from normal sadness in several ways. Human beings are not designed to be happy all the time (despite what society may suggest to us!) and sadness is a natural experience that comes with being human. Sadness differs from depression in several notable ways. First, with sadness there is an identifiable trigger: such as a break-up, being fired from a job, or failing a test. When we’re feeling sad, we will also often still be able to complete our essential daily tasks, even though productivity may suffer. Sadness also goes away with time. When I tell someone they are clinically depressed, it means that they’ve been feeling consistently down for at least 2 weeks nearly every day, and/or activities they once enjoyed no longer interest them. There may be no identifiable trigger for depression, and it comes with significant impairment in our day to day functioning—such as being unable to attend school or get up for work.
Alongside this problem, there’s a host of other issues, such as changes in sleep, increased feelings of guilt and worthlessness, and difficulty thinking, concentrating, and doing daily activities. In more severe cases, people with depression may also be experiencing suicidal thoughts. If you’re having suicidal thoughts, it’s important to talk to a medical professional as soon as possible to get the proper help in working with depression. While sadness and depression have significant overlap in how you feel, sadness typically does not require the level of intervention that depression might, since it often resolves on its own. Sadness can feel similarly distressing but perhaps more straightforward, with a clear exacerbating situation. While there's no timeline for feeling better, it may be worth seeking help if your sadness is significantly impacting your ability to do your daily responsibilities and feels more mysterious.
TIP OF THE WEEK
Learn the Skill of Values-Based Behavioral Activation
As a practitioner of CBT and ACT, I remind my clients with depression that simply attending weekly meetings with me isn’t the main mechanism of change and symptom reduction. More importantly, what they do with the information we talk about together and what they practice outside the therapy room is what helps them feel better. I encourage behavior change, while helping clients accept the initial discomfort that comes with activating ourselves. The initial effort required to clean the dishes after several days can feel pretty big, but the payoff at the end is oftentimes a feeling of accomplishment, which can fuel us to engage in other effective behaviors. I tell many clients about one of the axioms I learned in my training: focus first on the behavior, and the thoughts and emotions will follow.
Putting this into practice oftentimes means starting with values-based behavioral activation . You can start with identifying certain things that matter to you personally—such as creating an art project, going for a bike ride, tidying your room, or going out to the movies. Using The Field Guide for Depression you can identify the underlying values associated with each activity; an interest in biking may mean you value being adventurous, focused, and persistent. As you identify your underlying value(s), you can explore other activities consistent with your values. If you like going for a bike ride due to the focused, adventurous, and persistent nature, additional activities may be attending a rock climbing gym or going for a hike. If you have a hard time thinking about something that matters to you right now, you can try the ACT technique of asking your past, non-depressed self, what matters to them.
If you look at the list of activities you write down and they all look boring, uninteresting, or exhausting, you’re not alone. Biases in our thinking, memory, and attention are common in depression. Viewing our list of activities in a critical and pessimistic manner is yet another way depression can manifest—it’s like wearing sunglasses with a red lens; you end up seeing the world in a different shade. Try doing what feels manageable while stretching yourself each day, recognizing the difficulty of what you are asking yourself to do. If you struggle with self-judgment and criticism, try taking a different perspective and speaking to yourself as if you were supporting a close friend or loved one.
As we continue to identify values-based activities and do our best to engage with them, we can try to “raise the volume” of our values-based self-talk . For instance, after cleaning your room and acting on your value of being orderly, you can steer your inner voice to recognize your accomplishment, such as “Cleaning my room took a lot of effort and while it was hard for me, I did something today that was aligned with my values and the type of person I want to be.” Reviewing some of the responses you’ve written down in the E xploring Your Values section of the field guide may help you deepen this dialogue. The more we cultivate this inner dialogue and acknowledge the ways we act on our values, the less space there is for the “doom and gloom” inner voice that often goes hand-in-hand with depression.
As you continue to learn how to cope with depression or support a loved one, remember that if you try techniques and tools and they don’t work for you—don’t give up! There’s a multitude of resources to help manage and treat depression, and with patience and persistence, you’ll find something that works for you.
CLINICAL CORNER
Learn an Assessment Used to Evaluate Depression
Think of depressive symptoms as a spectrum. The more depressed you are, the more important it is to seek out more involved care. If you’re so inclined, google the Patient Health Questionnaire or the “PHQ-9,” one of the most commonly used screening tools for depression .
The PHQ-9 breaks down depression into several distinct categories: no depression, mild depression, moderate depression, moderately severe depression, and severe depression. People with “clinical depression” typically have a score of at least 10 on the PHQ-9. Self-help books, the field guide , and other approaches can be beneficial for folks in the mild or moderate range of depression. If your score on the PHQ-9 is above a 15, then you would probably benefit most from seeking out therapy or medication, as that’s when depression is considered “moderately severe” and a more involved approach may be most beneficial.
Each item on the PHQ-9 measures a particular symptom associated with the diagnostic criteria listed in the DSM-5 for major depressive disorder. In therapy, these diagnostic criteria are evaluated verbally at the initial session. The PHQ-9 is a helpful tool to figure out where you fall on the depression spectrum, and may help you identify what steps you need to take to tackle your depression.
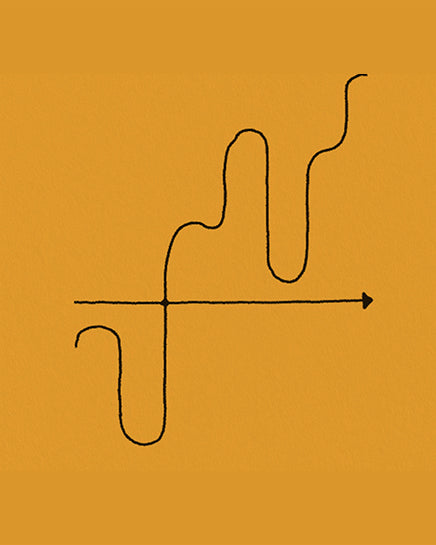
Another great use of the PHQ-9 is to measure your score weekly, bi-weekly, or monthly, and track the overall trajectory of change over two to three months. If your scores are getting lower—great! What you’re doing is working. If your scores aren’t changing or getting higher, it’s probably best to seek out a more involved approach compared to what you’ve been doing so far. This is something called progress monitoring a tool that many CBT clinicians use. It’s a helpful way to measure progress not only from a client’s self-report, but also in a more objective manner by using the PHQ-9 at periodic intervals throughout treatment.
Evaluating improvement in our wellbeing is tremendously helpful in directing our future efforts. Remember that different tools work for different people, so if your scores aren’t changing don’t stop trying. It just means that this particular approach doesn’t seem to be working for you. Try something else and see how it works!
Emory Strickland is a licensed clinical psychologist in Washington State. He specializes in providing evidence-based treatment for an assortment of anxiety disorders and has extensive experience in Cognitive Behavioral Therapy (CBT) and Acceptance and Commitment Therapy (ACT). He’s passionate about helping others overcome their life challenges and sharing the many research-backed tools and techniques that help people overcome anxiety.
Subscribe or contribute to Waiting Room.
This article is not therapy or a replacement for therapy with a licensed professional. It is designed to provide information in regard to the subject matter covered. It is not engaged in rendering psychological, financial, legal, or other professional services. If expert assistance or counseling is needed, seek the services of a competent professional.